Understanding treatment options and conditions empowers patients to actively participate in their own healthcare decisions. It allows informed choices that align with his/her personal preferences, values, and goals.
– Avista
Description of Vascular Surgery

Vascular surgery is a surgical specialty that focuses on the treatment of conditions affecting the blood vessels, such as arteries and veins. These conditions can include arterial blockages, aneurysms, and varicose veins, among others.
During a vascular surgery procedure, a vascular surgeon will make an incision in the affected area and use specialized tools and techniques to repair or remove the damaged blood vessels. This may involve inserting stents or grafts to open up blocked arteries, removing a blood clot, or repairing a weakened or enlarged artery.
Vascular surgery may be performed using traditional open surgery techniques, which involve making a larger incision, or minimally invasive techniques such as endovascular repair, which use small incisions and specialized tools to access and treat the affected blood vessels.
Vascular surgery can be performed for a variety of reasons, including to improve blood flow to organs or limbs, reduce the risk of stroke or heart attack, or relieve pain and other symptoms associated with certain vascular conditions.
Recovery from vascular surgery can vary depending on the individual and the specific procedure performed. In general, patients may experience some discomfort and limited mobility immediately following treatment, but can expect to gradually return to their normal activities with the guidance of their healthcare provider.
If you are experiencing symptoms of a vascular condition or have been diagnosed with a vascular condition, you must speak to a board-certified health-care professional to learn more about your treatment options, including vascular surgery, and what to expect before, during, and after the procedure.
Types of treatments done by a Vascular Surgeon

Vascular surgeons specialize in diagnosing and treating diseases of the vascular system, which includes arteries and veins. Some of the most common procedures conducted by vascular surgeons include:
- Endovascular procedures: This type of procedure involves using a catheter to access the blood vessels, usually through a small incision in the skin. Examples of endovascular procedures include angioplasty, stenting, and embolization.
- Open surgical procedures: In some cases, open surgery may be required to treat a vascular condition. This type of procedure involves making an incision in the skin to access the blood vessels. Examples of open surgical procedures include bypass surgery, aneurysm repair, and vein stripping.
- Minimally invasive procedures: Some vascular surgeons use minimally invasive techniques to treat vascular conditions. These procedures use smaller incisions and specialized instruments to reduce the amount of trauma to the body. Examples of minimally invasive procedures include endovenous laser treatment (EVLT) for varicose veins and radiofrequency ablation (RFA) for peripheral artery disease.
- Diagnostic procedures: Vascular surgeons may also perform diagnostic tests to evaluate the vascular system. Examples of diagnostic tests include ultrasound, CT scan, and angiography.
The specific procedures a vascular surgeon may perform depend on the individual patient’s condition and needs. Vascular surgeons work closely with other healthcare providers to provide a comprehensive treatment plan tailored to the patient’s specific needs.
Description of Interventional Radiology

Interventional radiology (IR) is a specialized field of medicine that uses image-guided procedures to diagnose and treat a variety of medical conditions. It is a minimally invasive approach that offers numerous benefits to patients compared to traditional surgery.
In interventional radiology, highly trained radiologists use advanced imaging technologies such as X-rays, fluoroscopy, ultrasound, and CT scans to guide small instruments or catheters through blood vessels or other pathways in the body. These procedures are performed through small incisions or puncture sites, avoiding the need for large surgical incisions.
Types of treatments done by an Interventional Radiologist

- Angiography: This involves the visualization and treatment of blood vessels using contrast agents (dyes) and X-ray imaging. It helps diagnose conditions like blockages, aneurysms, and vascular malformations.
- Angioplasty and Stenting: In this procedure, narrowed or blocked blood vessels are widened using a small balloon attached to a catheter. A stent, a tiny mesh-like tube, may also be placed to keep the blood vessel open.
- Embolization: It is a technique used to block or reduce blood flow to abnormal blood vessels or tumors. Small particles or special substances are injected to cause the vessels to clot or shrink.
- Biopsy: In interventional radiology, biopsies can be performed by using imaging guidance to precisely target and extract tissue samples for diagnostic purposes.
- Drainage and Abscess Treatment: Fluid collections or abscesses can be drained using image-guided techniques, relieving symptoms and preventing further complications.
- Tumor Ablation: This procedure involves the use of heat, cold, or other techniques to destroy tumors or cancer cells. It is an alternative to surgery for certain cancers and can be performed with high precision.
- Vertebroplasty and Kyphoplasty: These procedures involve injecting cement-like materials into fractured vertebrae to stabilize them and relieve pain caused by spinal compression fractures.
Interventional radiology procedures are generally less invasive, have shorter recovery times, and carry a lower risk of complications compared to traditional surgical methods. They often result in minimal scarring, reduced pain, and a faster return to normal activities.
It’s important for patients to discuss with their healthcare provider if interventional radiology is a suitable option for their specific condition. The interventional radiologust will evaluate their medical history, imaging studies, and symptoms to determine the most appropriate procedure. The patient’s active involvement and understanding of the procedure and its potential benefits and risks are essential for shared decision-making and achieving the best possible outcomes.
Description of an Abdominal Aortic Aneurysm (AAA):
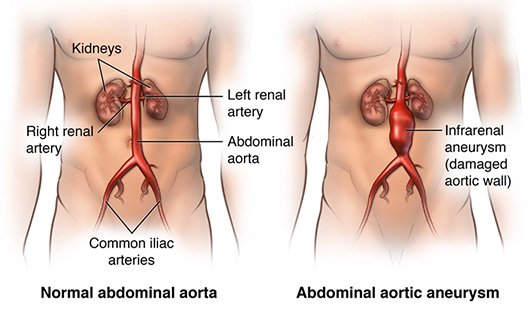
An abdominal aortic aneurysm (AAA) is a bulge or swelling in the wall of the aorta, which is the largest blood vessel in the body. AAA can be a serious condition, as the aneurysm can rupture and cause life-threatening bleeding. Therefore, it is important to diagnose and treat AAA as early as possible.
Risk factors for AAA include age, gender (men are more likely to develop AAA), smoking, high blood pressure, a family history of the condition, and atherosclerosis (a buildup of plaque in the arteries).
Treatment options for AAA depend on the size of the aneurysm and the patient’s overall health. Small aneurysms may be monitored with regular ultrasounds and lifestyle changes such as quitting smoking, managing blood pressure, and exercising. For larger aneurysms or those that are growing, medical interventions may be needed. These may include:
- Open surgery: a surgical procedure in which the surgeon makes an incision in the abdomen and replaces the damaged section of the aorta with a synthetic graft.
- Endovascular aneurysm repair (EVAR): a minimally invasive procedure that involves inserting a catheter with a synthetic graft through a small incision in the groin and guiding it to the site of the aneurysm. The graft is then expanded, sealing off the aneurysm and preventing further expansion.
Before the procedure, the healthcare provider will evaluate the patient’s medical history and perform a physical exam to determine the best treatment option for the patient. Patients may also undergo imaging tests, such as computed tomography (CT) scans, to assess the size and location of the aneurysm.
During the procedure, the patient may receive general or local anesthesia to numb the affected area. For open surgery, the surgeon will make a large incision in the abdomen and replace the damaged section of the aorta with a synthetic graft. For EVAR, the surgeon will make a small incision in the groin and guide a catheter with the synthetic graft to the site of the aneurysm.
After the procedure, patients may experience some discomfort and swelling in the affected area. The healthcare provider may recommend pain medication and compression stockings to reduce discomfort and promote healing. Patients may also need to avoid certain activities, such as heavy lifting and strenuous exercise, for a few weeks after the procedure.
In conclusion, abdominal aortic aneurysms are a serious condition that requires prompt diagnosis and treatment. If you are at risk for AAA or are experiencing symptoms, you can to a healthcare professional to learn more about your treatment options and what to expect before, during, and after the procedure. With the right care and management, patients can reduce the risk of complications and improve their long-term outcomes.
Description of Kidney Disease:

Kidney disease, also known as renal disease, refers to the condition where the kidneys are damaged and cannot function properly. The kidneys play a crucial role in filtering waste and excess fluid from the blood, producing urine, regulating electrolyte balance, and maintaining overall body health. When kidney disease occurs, these functions are impaired, leading to a buildup of toxins and fluid in the body, which can cause various complications.
There are several types of kidney disease, including:
- Chronic Kidney Disease (CKD): This is a long-term condition where the kidneys gradually lose their function over time. CKD is often caused by conditions like high blood pressure, diabetes, or certain kidney infections.
- Acute Kidney Injury (AKI): AKI is a sudden and severe decline in kidney function. It can occur due to factors such as dehydration, infections, medications, or decreased blood flow to the kidneys.
Treatment options for kidney disease depend on the underlying cause, the stage of the disease, and the specific symptoms. Here are some common approaches:
- Medications: Depending on the type of kidney disease, medications may be prescribed to control blood pressure, reduce protein leakage in the urine, treat infections, manage diabetes, or alleviate specific symptoms.
- Dietary changes: A kidney-friendly diet is often recommended, which involves limiting sodium, phosphorus, and potassium intake. This helps ease the workload on the kidneys and maintain proper electrolyte balance.
- Fluid management: Monitoring and controlling fluid intake are essential to prevent fluid retention and swelling. Your doctor may provide guidance on how much fluid you should consume daily.
- Dialysis: In advanced stages of kidney disease, when the kidneys can no longer adequately perform their functions, dialysis may be necessary. Dialysis is a medical procedure that involves using a machine to filter waste and excess fluid from the blood.
- Kidney transplant: For some patients with end-stage kidney disease, a kidney transplant may be considered. This involves surgically replacing the damaged kidney with a healthy kidney from a donor.
Several risk factors increase the likelihood of developing kidney disease, including:
- Diabetes: High blood sugar levels can damage the kidneys over time.
- High blood pressure: Uncontrolled hypertension can damage blood vessels in the kidneys.
- Family history: Having a family member with kidney disease increases the risk.
- Age: The risk of kidney disease increases with age.
- Smoking: Smoking can worsen kidney damage and increase the risk of kidney disease.
- Obesity: Excess weight can strain the kidneys.
- Certain medications: Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) or other nephrotoxic medications can harm the kidneys.
It is important to note that early detection and intervention are crucial in managing kidney disease effectively. Regular check-ups, maintaining a healthy lifestyle, and managing underlying conditions can help reduce the risk of kidney disease or slow its progression. If you have concerns about your kidney health, it is best to consult with a healthcare professional for proper evaluation and guidance.




